







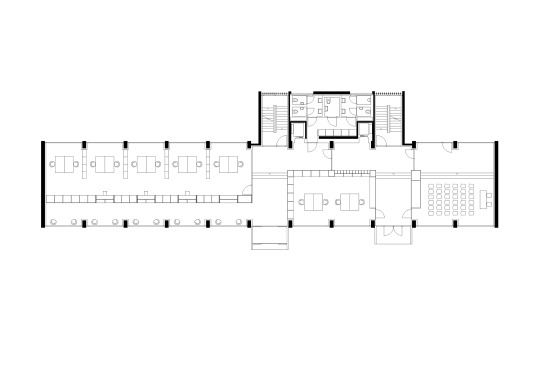
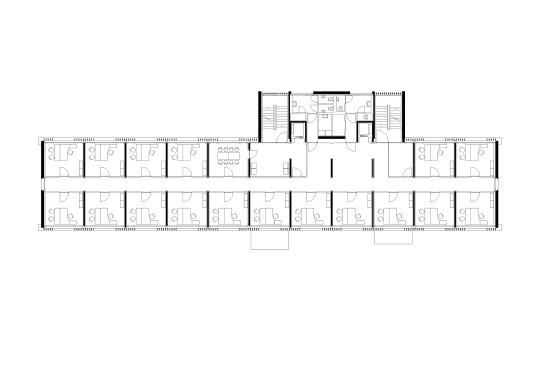
Durisch & Nolli - Stabile administrative building, Lugano 2019. Photos © Studio Willen.



Insomnia is a uniquely vexing medical problem. It is the most common sleep-related issue, thought to affect around 10-40% of the population in the US. So it is a challenge that affects a whole lot of us.
Yet despite its prevalence, options to manage the condition are lackluster at best. Pharmaceutical interventions for insomnia are not helpful for many patients, and the chronic use of these medications comes with really nasty side effects. We know, for instance, that chronic use of these medications is associated with elevated risk for Alzheimer’s disease.
Why is there such a paucity of good treatments? Perhaps because it remains rather poorly understood. Insomnia has been known and documented for thousands of years, but it has proven to be difficult to study for a number of reasons. It’s hard to develop good animal models for the condition, it’s tricky to objectively define (though there are some genetic and molecular models associated with it), and symptoms manifest quite differently between individuals. Additionally, there are often strange discrepancies between patients’ self-reported sleep quality and results from objective sleep measures obtained in a lab setting (like polysomnography).
In order to address a complex disorder like insomnia, we need to get to the root cause. For most of us, it is clear that the origin lies within the brain. This has compelled some very clever researchers to take snapshots inside the heads of patients with insomnia (via positron emission tomography, or PET), and compare them to normal controls. The results of such studies have been enlightening.
And that brings me to our guest for this episode.
In this episode of humanOS Radio, Dan speaks with Eric Nofzinger. Dr. Nofzinger is a renowned expert in the science of sleep, and formerly the president of the Sleep Research Society. He spent more than 35 years practicing sleep medicine and studying the neurobiology of insomnia at the University of Pittsburgh School of Medicine.
As a researcher at Pittsburgh, Dr. Nofzinger frequently interacted with patients with insomnia. They would often attribute their inability to sleep to a “racing mind.” If you’ve ever had trouble falling asleep due to incessant rumination, that characterization probably sounds pretty relatable. Furthermore, they would often claim to have hardly slept at all, even when polysomnography showed that they had experienced normal sleep.
He, along with other scientists in the field, suspected that there was a biological basis for these commonly reported complaints. To gain meaningful insight into what was going on, he couldn’t just look at sleep patterns – he needed to look inside the brain. To that end, he started conducting functional imaging studies on patients with insomnia to examine patterns of brain activity and metabolism during sleep.
In one such trial, subjects completed regional cerebral glucose metabolic assessments while awake and while asleep using the FDG PET method. These scans were telling. During normal healthy sleep, there are typically substantial reductions in brain activity, particularly in the frontal cortex. But imaging for individuals with insomnia painted a very different picture. Their brains remained comparatively active during sleep, particularly in the frontal cortex, and they exhibited greater cerebral glucose metabolism during sleep and while awake. So, when these people claimed that their minds were racing throughout the night – when their brains should have been resting – that was actually a remarkably accurate assessment.
These kinds of studies demonstrate that insomnia is, in essence, a disorder of hyperarousal of the brain. With this revelation, what can be done to slow down the racing mind?
Cooling it down. 
It has been known for some time that application of a cooling stimulus to the head can lower the brain temperature in the underlying cortex, and in turn reduce brain metabolism. This insight led to the development of Ebb, a sleep therapy unlike any other that has yet been invented. Here’s how it works: the device is comprised of a headband attached to a bedside unit. Cold fluid circulates through the forehead pad from the bedside unit, keeping your forehead at a cool temperature throughout the night. In this way, Nofzinger and his colleagues hope to target the root cause of insomnia, calming the mind and body.
To learn more about Ebb and Dr. Nofzinger’s research, check out the interview!
On Soundcloud | Spotify | Apple Podcasts | Google Play | Stitcher | iHeartRadio | Overcast.fm | YouTube
Have you considered becoming a Pro member of humanOS.me? It costs just $9.99 per month, and when you go Pro, you get access to all our courses, tools, recipes, and workouts. Pro members also support our work on blogs and podcasts, so thanks!
If you think other people would benefit from listening to this show, you can help us spread the word by leaving a review at iTunes. Positive reviews really help raise the profile of our show!
| Eric Nofzinger: | 00:00 | In terms of helping people get the sleep, we feel we’re in the same ballpark in terms of efficacy is what a hypnotic might be and also that Cognitive Behavioral Therapy is in the same range. |
| Dan Pardi: | Hello everyone. Welcome back. Today I’d like to welcome professor Eric Nofzinger to humanOS Radio. Dr. Nofsinger is a renowned expert in the science of sleep and formerly the president of the Sleep Research Society. He spent more than 35 years practicing sleep medicine and studying the neurobiology of insomnia at The University of Pittsburgh School of Medicine. | |
| 00:14 | Now, insomnia is a vexing problem. Most comments sleep-related issue thought to affect around 10 to 40% of the population. It’s been known and documented for thousands of years and yet it’s been proven difficult to study. It’s hard to develop a good animal model for it and the symptoms manifest differently in individuals and it’s hard to effectively define. Although there are a few genetic or molecular markers associated with the condition, so perhaps it’s not surprising that treatments for insomnia have been somewhat lackluster. Pharmaceutical interventions for insomnia are not helpful for many patients and the chronic use of them comes with some really nasty side effects. We know that the chronic use of these meds associated with an elevated risk for Alzheimer’s disease. | |
| And so as a researcher at Pittsburgh, Dr. Nofsinger performed functional neuro imaging study on patients with insomnia where he revealed the differences in brain activity and brain metabolism both while asleep and while awake, or interacted with them, you’d often attribute their ability to sleep to a racing mind. If you’ve ever had trouble sleeping, you might be able to relate to that. | ||
| He eventually hypothesized that a major cause of insomnia was hyper activity in the frontal cortex, when this part of the brain is less active, a person is more likely to fall asleep and were likely to experience restorative sleep. From his insight he developed Ebb a medical device that reduces activity in this part of the brain and thus counter racing mind. So we’re going to talk about that today. So first Eric, welcome to humanOS Radio. | ||
| Eric Nofzinger: | Well, thank you very much. It’s a great pleasure to be here. And what a nice introduction. You’ve summarized everything very nicely. Thank you. | |
| Dan Pardi: | Wonderful. To begin, I would love to hear more about your research interests. How did you get into sleep and how did you gravitate towards insomnia and the work that you’re doing with imaging? | |
| Eric Nofzinger: | 01:54 | You know, it’s been a lifelong journey. The running joke is that this is one of the longest overnight success stories in the district because it has taken me my entire life to get to the point where I’m at now. My interest really began back when I was actually an undergraduate student. At that point in time I had an interest in human behavior, more specifically, what is it that goes wrong when individuals have mental health problems, depression, anxiety when they don’t feel well and then trying to understand how to improve behavior, what are the ways that we can we help individuals? |
| I had actually taken a course in Dream Psychology of fall things as part of an undergraduate major in Psychology. And at that point in time I became aware that the dream material was very important in understanding who we were, how we did things, how we feel about things, and if we could understand that better, we might be able to help people in their daily lives. | ||
| 02:00 | So that was kind of my first understanding that whatever it was that was happening to us when we were asleep at night time, well, whatever cognitions or mental content or brain activity, it was extremely important to who we were and how we function during the daytime. | |
| I followed up that interests, went to medical school, continued an interest in psychiatry, learn more about formal assessment, diagnosis and treatment of psychiatric patients and continued an interest in sleep, got involved in sleep research even as a medical student. And then as I was searching for residency training, I went to the University of Pittsburgh, which was a leader in sleep research and psychiatric disorders as well as in the area of sleeplessness and insomnia. | ||
| 02:09 | During my time at the University of Pittsburgh, I began a formal research career and was a student with some of the best methodological researchers in the field. At that point in time, I had access to tremendous resources in terms of asleep lab, patient populations, other investigators to work with can learn much more about the methodology of sleep. | |
| I learned at that point in time much more about the relationships between specific psychiatric disorders and their sleep at nighttime. How does sleep get disturbed and various disorders, and then how does that impact treatment? If we can help individuals sleep better at nighttime, it was very apparent that, that was part of the process of recovery for them. | ||
| There were some limitations, however, in all of the research that was being conducted at that point in time, we mostly relied as did everybody else on just looking at the EEG at nighttime and from that we can look at sleep staging. What are the different stages of sleep that somebody goes through at night and time? What’s the pattern, what’s the timing of that, what’s the intensity of the different stages of sleep? And then how does that relate to clinical course, their likelihood of responding or not responding to different types of treatments? | ||
| It was kind of an imprecise tool, if you will. There’s only so much that the EEG and sleep staging can tell us about what’s really happening in our minds and in our brains during sleep. About this time I learned about other techniques for understanding brain function through functional neuroimaging. Back in the 80s and 90s it was considered the decade of the brain and at that point in time there was an explosion of research methodology and research findings using functional neuroimaging techniques, either X-ray techniques, CT scans, functional MRI, positron emission tomography, using these ways of looking at activity in the brain, we were finding out much more information about how the brain operates, what are the different parts of the brain that become involved in different disorders and then how do we alter that. | ||
| At that point in time, I was one of the first individuals and like to think of myself as a pioneer in the area of applying functional neuro imaging to the study of the sleeping brain. There had been lots of individuals interested in studying wakefulness, but not a lot of people had applied it to the issue of sleep. And there’s some particular challenges associated with that. It’s very hard to have an individual sleeping in a scanning environment. And so that was a challenge. | ||
| So we had to develop novel methods using pet techniques. We could actually have an individual fall asleep in a comfortable bedroom environment and we could inject a radiotrace and then take them to a scanner at a later time point because the image was kind of frozen in time at the time that they were in their bedroom. And using those types of methodologies, we could figure out what parts of the brain were active during dreaming sleep. What were the parts of the brain that were responsible for all the wonderful stories, images and fascinating mysteries of the mind during rapid eye movement sleep. | ||
| And then if we turn the camera and focused on non-REM, we could find out the different areas of the brain that were more responsible for the deeper, more restorative aspects of sleep that we typically think about in stage three and four sleep. So that’s a little background into kind of my early trajectory and how I got started in looking at the brain mechanisms to sleep. | ||
| Dan Pardi: | To summarize, a lot of sleep research has been conducted with polysomnography, which is a multiple measures of sleep. One of the main aspects of that is electrodes in the brain, so it’s trying to read brain wave activities from the outside of the skull. It does give us insight into clinical conditions, but your work was looking at imaging where we had deeper resolution into how the brain was working and you were looking specifically at these states during a sleep state, the activity of brains during different stages of sleep, which was normal. Before we get into some of the imaging work, how common is insomnia? | |
| Eric Nofzinger: | There are multiple categories, but the most common abnormality we actually think of as sleeplessness, there’ve been lots of large scale community wide studies done and sleeplessness, which is occasional trouble falling asleep, staying asleep or having a restorative sleep at nighttime. That can impact more than half the population. And so the raw numbers, we always screw out numbers like 150 million individuals in the United States or more and even more worldwide, so it’s the inability sleep soundly at nighttime, at least on an occasional or in transit basis. It’s a universal issue and it’s extremely widespread. | |
| If you dive down into medical disorders, things that medical community might think of more severe cases, it’s still is probably 20% to 25% of the population, so we’re still talking about 50 million or more individuals in the United States that have more severe incapacitating sleeplessness beyond what the usual person might experience. | ||
| Dan Pardi: | With your imaging work, what were you able to detect that polysomnography was not able to see? | |
| Eric Nofzinger: | People that are having difficulties sleeping at night time. One of the things platonically that these individuals report is, I can’t get my brain to shut off at nighttime. I don’t feel like I’m sleeping. So there’s this subjective feeling that individuals have that my mind and my body are just not shutting down when I go to sleep at nighttime. We knew from imaging studies in healthy individual that in order for somebody to get deep restorative sleep at night time, there had to be both whole brain reductions and metabolic activity, but more selectively in parts of the neocortex and especially in the frontal cortex. The frontal cortex had to show very large reductions in metabolic activity. | |
| 07:51 | If we think about it, the frontal cortex is our executive brain. That’s what part of our brain that we use most during the daytime. If we’re thinking about things, if we’re trying to problem solve or ruminating about things. The part of our brains that we’re using right now, we’re, I’m giving a small talk, I’m trying to remember things, the listeners are trying to integrate this with past information in their lives. When we’re awake, the prefrontal cortex, the frontal cortex or executive mind is extremely busy. It’s just the contrast during sleep, so that part of the brain really goes offline. | |
| The way I like to think about it is almost like if you’re working out a muscle, if you workout a muscle very hard during strenuous exercise, the muscles that we’re working hard really need to rest and recover the most. The brain in a simplistic sense works the same way. Frontal cortex is active during the daytime with all of our thinking and conscious activity and that’s the part of the brain that needs to rest the most and shut down when we go to sleep at nighttime. | ||
| 08:22 | What we’ve found in individuals who are not getting good sleep at night is that, that doesn’t seem to be happening, so there’s this contrast. The more individuals had a tendency to have arousals or awakening across the nighttime, the more their frontal cortex seem to be engaged. And indeed we correlated the amount of wakefulness that somebody was having across the nighttime with metabolic activity across the brain and found that the frontal cortex was one area of the brain where it seemed to continue to be running throughout the nighttime and that seemed to correlate with the individuals complaints that my mind isn’t shutting down, it’s not resting at night time, and we think that hurt or that resides in the frontal brain or in the frontal cortex. | |
| Dan Pardi: | I spoke with Kristen Wilkins on the podcast. One of the things that we discussed was the usage dependency of the depth of sleep depending on how active the brain was during the day. What I’m hearing from you is that people that tend to have that racing mind at night while they’re sleeping, this part of the brain that should be resting because it was active and awake and being used all day. It has higher level of activity than what you would see in patients brains that don’t have insomnia. | |
| Eric Nofzinger: | That’s absolutely right, and then the flip side of that is what happens during the daytime in these individuals, we know that one of the functions of sleep is make us feel rested. It’s for the purpose of getting rest so that when we wake up the next day, we’re fresh, we’re ready to go, and we’re ready to start working hard. But in contrast and in individuals with insomnia because her brain is working hard at nighttime, especially on the frontal cortex, we also found that when we did imaging studies of the brain in individuals with sleeplessness during the day time, they had less activity in the frontal cortex. | |
| 09:28 | So one of the detriments of sleep deprivation is that the frontal cortex doesn’t function as well during the daytime. When we think that that relates to their clinical complaints, that they can’t concentrate, they don’t feel refreshed, they don’t feel alert, energetic during the daytime, they can’t focus and function as well during the daytime. So it’s an inability to get that rest that they need at night time, it’s not being restored, and so then it becomes deficient and impairs somebody’s daytime waking function. | |
| Dan Pardi: | A lot of people can relate to that. Everybody’s had a little bit of insomnia at some point in their life and can recognize the feeling of madness that you can’t sleep when you’d like to, and the feeling of mental fatigue and tiredness and frustration the next day as a result of the lack of sleep. Let’s talk about Ebb now. So this is a company that you’ve started. When did the company begin? | |
| Eric Nofzinger: | 09:35 | The company was officially formed in 2008 so it’s a small startup company. At that point in time, I was the only employee in the company for a couple of years, so it’s been around for awhile. |
| Dan Pardi: | What is the product that you have now? | |
| Eric Nofzinger: | Based on a lifelong history of treating patients and then also trying to understand the brain mechanisms, what causes their sleep difficulties at night time. And then as a practicing clinician, I was very familiar with the treatments that existed 10 years or so ago. In the medical community, really the only thing that doctors have to fall back on are the prescription medications, the hypnotic medications, things like Ambien, Lunesta, Halcion, Doralmine, Restoril So all of these medications have been known to the medical community. They’re known to patients and it’s known that they’re effective. They do help individuals sleep better at nighttime. | |
| But the problem that I kept hearing from both doctors and patients is that these are not great solutions. The biggest problems, and this has been recognized by the Food and Drug Administration, they’re most concerned about the issues related to drowsy driving. And when somebody gets up in the morning, they still may be under the influence of the medication they get on the road, they could get into an accident. | ||
| So that’s one problem of the medications. Very difficult. Once a patient gets on these medications to, for them to get along a difficult long journey to try to wean them off of medications if they might to get them off with them at some point in time, they also have significant problems to impairing memory formation. They can cause balance problems. | ||
| 12:21 | So the world of medicine was in a funk at that point in time. It’s like got these patients and there’s millions and millions of them. Lots of them coming into my office. But I can’t tell them that I’ve got a great solution. Based on the imaging work, I started to wonder, is there a different way that we can start to manage these individuals? Is there a safer alternative that works on the specific problems in the brain that individuals with sleeplessness might have? | |
| I knew that frontal cortex was important for deep restorative sleep. I knew that individuals with sleeplessness were not able to kind of get that part of the brain to settle down. So I started brainstorming is to what are some potential ways that I might through some kind of external safe mechanism get the brain to settle down in the frontal cortex. And I think somewhere on the back of my mind, through my medical training, I hadn’t become familiar with the concept of Cerebro hypothermia, which is cooling brain tissue for a long time in other disciplines in medicine, emergency medicine, neurology, neurosurgery, cardiothoracic surgery. If you can cool brain tissue, you can protect brain tissue. It’s a good thing for the brain to have reduction in temperature, it reduces metabolic activity and it reduces a lot of the toxic effects that might come about through hypoxia or brain injury that might otherwise happen. | ||
| 12:47 | So the concept of cerebral hypothermia hadn’t been around but it had never really been applied to the management of sleep disorders and specifically with individuals who weren’t sleeping well at night time. So the regional focus then was is there some way we can get some type of a cooling stimulus into the frontal cortex of the brain, it facilitate the natural reduction in activities that shouldn’t happen in individuals with sleeplessness. | |
| I wrote and was funded for a small development grant to produce a little medical device and the purpose of the device was to basically cool the forehead. The forehead overlies the frontal cortex and the initial device was a very simple circulating fluid pad connected to a laboratory grade water bath and we were able to change the temperature across the wide variety of spectrums to get the temperature that we thought was safe, effective, and was helpful for individuals. | ||
| The first testing that we did with this device was a brain imaging study. As a scientist, I needed to know, can I really change brain function in this manner? I wanted to know that answer before I started taking it into clinical trials. | ||
| Dan Pardi: | 13:57 | Right. |
| Eric Nofzinger: | So when I was still at the University of Pittsburgh, the first study that we did was an imaging study where we looked at the impact of the device over the forehead, cooling the forehead, and we did find through looking at pet studies that it reduce metabolic activity in the frontal cortex during sleep in individuals. And then when I talked with the people who participated in the study, I got some really wild reports about their sleep and many of them said, “I’ve never slept like that before.” And they hadn’t found themselves being able to drift into kind of a deeper, more restorative sleep and being able to stay asleep for a longer period of time. That was surprising to them because they hadn’t experienced that before. | |
| 14:16 | The ultimate hope is that not only is there a mechanism but we also might be able to improve the lives of individuals. So that was the hope and it was nice to know that I didn’t have to do all kinds of fancy physiological tests. I just talk with the individuals after wearing the device and I said, “This thing seems like it’s helping me.” So from there then we did some additional studies where we played around with the actual temperature ranges to figure out some precise temperatures that were in a very comfortable range but also still had kind of maximum activity on being able to help with sleep at nighttime. | |
| We did some dose ranging studies, if you will, across the variety of different temperatures. We found the temperature that seemed to be the most helpful and then we took that into larger scale clinical trials. And then we were able to demonstrate actually on an FDA application for clearance that the device did improve sleep and individuals with sleeplessness. | ||
| Dan Pardi: | 14:28 | For people that are trying to imagine what this looks like. Explain the experience of using Ebb. How does it fit into the body? What does it look like for you? |
| Eric Nofzinger: | For individuals that are interested in learning more about it, we do have a website where pictures of the device and more description. It’s www.ebbsleep.com but in a general sense, there are kind of three components of the device. There’s a bedside cooling unit. Inside the cooling unit is a cooling chamber that cools some circulating fluids and then from the bedside unit to the forehead pad there are some tubes that carry the channels of water and then the water circulates through channels in a forehead pad that’s slipped on, just like you were putting on a baseball cap or a bandana, if you will. It’s a very comfortable and flexible forehead pad. Very thin probably a centimeter or in depth. | |
| 14:30 | The fluid channels are in a plastic lining and then on the top of that is a comfortable material. That’s a headband that holds the fluid channels on the forehand and a class behind the hat and you can adjust it according to comfort. So an individual when they’re getting ready to go to bed at nighttime, there’s the bedside unit and the headband, or they can sit on the side of their bed, slip the device over their forehead, just like they were putting on a hat and there’s a dial on the machine. You push the dial in to start the cooling and the pump action. The circulating begins, the cooling begins, and over the next 10 to 15 minutes, the fluid in the channels will start to cool down. | |
| What people find is as it starts to cool down. In the first 10, 15, 20 minutes or so of wearing the device, there’s a very calming relaxation, almost meditative, the spa like experience that they start to feel. This may be related to the frontal cortex starting to go offline, if you will. There’ve been lots of imaging studies of meditation, for example, where when you start to take the frontal cortex offline, you get this kind of very positive, almost transcendental experience. | ||
| So there’s a relaxation effect that people start to have and then they start to disconnect a little bit from the world around them, kind of a pleasant way, the thoughts that might been distracting them during the daytime kind of start to filter away and drop away. And that’s the initiation of the process of being able to fall asleep. | ||
| So usually within 10, 15 minutes, that experience starts to take hold and then individuals lay down and they sleep with the device on throughout the nighttime and then on awakening the next morning they can take it off and turn the device off. So for the usual case scenario, we do recommend that individuals put it on maybe about 20 to 30 minutes during a wind down period that before actually they want to fall asleep. Then they leave it on throughout the nighttime and then take it off in the morning when they get up and want to go about their day. | ||
| Dan Pardi: | When you put it at a particular temperature. And by the way, for these users that are visualizing this, imagine the eye mask. It looks a lot like that, but it’s worn on the forehead instead of over the eyes and it’s got a tube that is coming out of it and that’s where the water circulates through it. That water has to circulate through so that it can continue to cool? | |
| Eric Nofzinger: | Correct. So you can imagine your body produces a lot of heat and especially the forehead produces a lot of heat and so you have to provide a continual kind of cool and stimulus to that to keep some type of mechanism in place. And people often wonder, can I just put an ice pack or something like that on. The problem there is that the body heats up, it melts the ice back and then you’ve got a slushy mess within about 20 to 30 minutes or so. Whereas this device is actively cooling across the nighttime and providing that thermal transfer to a degree that you can’t get with for just using something that comes out of the refrigerator or the ice pack. | |
| Dan Pardi: | It almost sounds like Craig Heller’s cooling device that was used to cool core body temperature from the hand for athletes. It says it’s got sort of water through. | |
| Eric Nofzinger: | Correct. | |
| Dan Pardi: | So what is the range of temperatures that this device could be set out? How much are you trying to actually cool to head with Ebb? | |
| Eric Nofzinger: | 18:47 | So the lower temperature or the coldest temperature, the way that we’ve found that is looking at a range of temperatures and there’s a temperature below which becomes uncomfortable. You’ve got to actually activate temperature pain receptors. I mean if you put an ice cube on, eventually it’s going to be painful. The low temperature for this device is 14°C, and that’s about the highest 50°F. So 56, 57°F. It’s not anywhere near ice cube temperatures. So that’s the lower range. |
| And then the upper range is 16° is in the low 60°F range. So the total range of the device is 14° to 16° degrees. And part of that was, part of the FDA. It was necessary to select some narrow range so that we can test the same temperature across many individuals. And an individual has the ability to change the temperature according to their personal preference across the nighttime. | ||
| Dan Pardi: | 18:47 | Had you tried utilizing a cooling device and other parts of body are trying to lower core body temperature versus directly cooling the forehead given its proximity to the frontal cortex? |
| Eric Nofzinger: | It’s a very interesting and important question. We did measure a core body temperature across the night time when individuals are using this device. If you start to lower core body temperature, people start to feel cold and that can actually be disruptive for sleep. So when we looked at core body temperature across the nighttime, there is no difference between using the device for not using a device well. It’s not a whole body thermal regulatory effects that the device seems to be happening. It does seem much more specific on the frontal cortex and the specific changes and we think it’s not so much at temperature change, but rather it’s reducing metabolic activity at the frontal cortex. | |
| The amount of temperature transfer is based on some neurosurgical models is probably less than 1°C, so at the surface of the cortex, at the surface of the brain. So it’s a very minimal amount of change and brain temperature that we think might be happening. And that’s physiologic in the sense that if you look at the normal circadian rhythm of brain temperature, it fluctuates by at least 1°C across the 24 hour period of time. | ||
| We think that we’re in a physiologic range of reducing brain temperature and reducing metabolic activity. And that’s important because we don’t want to cause any potential side effects. We want the device to be safe. | ||
| Dan Pardi: | 20:30 | Do you envision a use case where even though this is needed for during sleep, it’s used Perry sleep to help get you into a better state for getting the sleep that you want? |
| Eric Nofzinger: | Great question. So there are different use case scenarios in the evolution of any product. One is what do you have to do to satisfy the FDA and what does the FDA allow you to do? You’d have to have some constant protocol and some constant application across all individuals in order to get clearance. Well once a product becomes available, people are curious and you just as you have pointed out, what if I use it in different times because they helped me here, does it help me there? Do I need to wear it all night long? We are becoming more and more familiar that there are individuals, they never really had trouble staying asleep across the nighttime. Really, they just needed help getting to sleep. For those individuals, they do use the device half an hour or an hour during that wind down period, but they don’t wear the device throughout the entire night and whatever works for individuals, we want people to feel comfortable playing around with the device, personalizing it, taking control of their therapy, if you will. | |
| 20:38 | So we have that scenario where people can just put it on prior to bedtime. We also have the opposite. People that never had any trouble falling asleep, but their main issue is, I wake up a lot at nighttime. So some people use it, they don’t put it on before going to bed, but they wait until they’ve had their normal one or two o’clock awakening. They put it on at that point in time and then they get kind of that calming relaxing effect and it makes it easier for them to get back to sleep in the middle of the night. | |
| Dan Pardi: | That was going to be one of my next questions since I think for chronic insomniacs sleep maintenance is more prevalent than sleep initiation. Can you wait until the sleep problem occurs and then you know you have an ACE in the hole, if you will, to help you get you back to sleep. It’s funny. That alone might actually help people sleep knowing that they’ve got something that can help them sleep. | |
| Eric Nofzinger: | I mean, now we’re getting into kind of the cognitive therapy of insomnia. They absolutely, there’s no question and we do have individuals who have episodic problems with insomnia where they don’t need something night after night, but somehow just knowing that this is there and that if they do have a problem and they can turn to it, it doesn’t give them the sense of control that I’m not helpless in my situation. I have something that I can turn to if I need to. | |
| Dan Pardi: | The world of bio hacking is now coming very popular where people are looking towards various strategies to optimize different physiological functions like sleep. Do you envision the possibility of the device being used? Not for insomniacs but to help people get deeper sleep at night so that they feel more restored? The same thing that those insomniacs reported but abnormal populations. | |
| Eric Nofzinger: | We have many individuals who otherwise reasonably normal sleepers who are learning about the product and I do believe that’s how number of individuals starting to think about it in that way. It’s kind of a performance enhancing product and another wise healthier individual is you know, it’s all the people that you’ve talked with, the work that you’ve done. The sleep is critical to a human performance on a variety of levels during the daytime. So trying to augment that is one strategy that some people have been using. We obviously haven’t done any large scale clinical trial to test out impacts on human performance in otherwise healthy individuals, but it wouldn’t surprise me that we’ll see more and more use like that. | |
| Dan Pardi: | I could imagine everybody having this on their bedside table. One use case is to use it before bed to try to get you into that zone ahead of time prior to bed. Nonclinical populations that have chronic insomnia might try to use it during sleep to have deeper sleep, that’s more sort of. Then you’ve got insomniacs who have a serious condition that is chronic. There needs something that’s not benzo or non-benzodiazepine, hypnotic clicking Ambien. That’s got to be serious side effects. We’ll talk about that more in a moment here and how Ebb compares and everybody of course experiences the occasional waking in the middle of the night and can’t go back to sleep because your mind starts to race. Having this on your bedside table and being able to put it on and increasing your chances of getting back to sleep and salvaging the last couple of hours can salvage your next day. That’s really exciting. | |
| 23:38 | Let’s talk about how this product compares in insomniacs to medication. What have you seen in terms of the clinical benefit of people that are using this device for their insomnia? | |
| Eric Nofzinger: | It’s a question that a lot of people ask. How does this compare with existing therapies? There are two existing therapies. One is medication and the other treatment for insomnia is Cognitive Behavior Therapy. There’ve been lots of studies in both of those categories, so we have very good understanding of the impact of these treatments on the ability to get to sleep and stay asleep and then how people feel during the day time. | |
| 23:55 | We wanted to make sure that we understood the impact of this device in the same world that these other treatments exist. What I mean by that is the way that they’ve demonstrated their efficacy is through polysomnographic sleep studies primarily if you looked at, if you measure somebody’s sleep at nighttime, so we wanted to do the same thing. When we were designing our trials for the FDA clearance process, we did the identical studies that the pharmaceutical industry might do for a hypnotic, so we looked at the traditional EEG measures of sleep. | |
| What we’ve found is that although we didn’t do a head-to-head comparison and we can’t make any director’s specific claims about how it matches up, we can look at literature references for what’s been published and there was one meta analysis on hypnotics that looked at all the FDA trials for lots of different drugs and that were submitted to the FDA and then they looked at the different effect sizes on various sleep parameters across these trials. | ||
| 24:34 | What we found is that our device fell out right in the middle of all of the hypnotic trials in terms of the effect size, so that’s one way that indirectly you can match up what one therapy would do in relationship to another. In terms of helping people get this sleep, we feel we’re in the same ballpark in terms of efficacy is what a hypnotic might be and also that cognitive behavior therapy is in the same range. | |
| We also have been able to show that on average individuals are getting about 60 minutes more sleep at nighttime with the use of the device and that’s across all of our patients and our randomized controlled clinical trial that was published about a year ago. So getting the sleep, staying asleep or getting somebody a total of about 60 more minutes of sleep at nighttime. And then we did an hour by hour analysis. The graph of that is in the published article on our clinical trial. There’s a large effect early in the night within the first couple of hours of the night where it increases the number of minutes of sleep, but it seems like there is a continuing benefit across the nighttime, each hour of the night has more minutes of sleep with the use of the device and that seems to be comparable to what we’ve seen with other hypnotic trials. | ||
| 24:42 | The place where it really differentiates is in the safety profile. This is a completely safe device. When we were talking with the FDA, they were very familiar with cooling applications and various parts of the body. They had no concerns whatsoever with respect to safety and across all of our clinical trials and we’re talking close to 4,000 patient nights use of the device very low incidents of side effects and nothing that differentiated it from the placebo conditions that we were using. | |
| So efficacy is in the same ballpark range as other treatments that are out there, be it medication or cognitive behavior therapy. The advantage here is the absence of the adverse events and we think of it as working more on the natural sleep-wake system. If you will. | ||
| Dan Pardi: | 24:43 | When did the product launch? |
| Eric Nofzinger: | We launched about a year and a half ago and we began with a prescription device that was cleared by the FDA and then we have more recently within the past few months have launched a consumer non-prescription device to help individuals with sleeplessness at nighttime. So we’re very early in that launch phase. Then we’re the enthusiasm and the interest that we’re seeing here is probably double what we thought we were going to get. So very excited about the launch into the consumer channel, which gives us the ability to impact all those individuals that don’t really want to go to a doctor to have their sleep problems taken care of and they may not want to start on medications that could potentially have some side effects. | |
| Dan Pardi: | 24:49 | So you don’t need a prescription for this. You can go right to ebbsleep.com and you can purchase one from there. |
| Eric Nofzinger: | Absolutely. | |
| Dan Pardi: | Do you plan to do more trials looking at the efficacy of Ebb in different types of insomnia or different types of populations? | |
| Eric Nofzinger: | 25:51 | We do. So we have a list of potential new things that we’re interested in and much of this comes from the experience now that the device has been out in the market and people using it for a variety of different things. We’re getting feedback as to where the device could also be helpful. The one area that’s prominent right now, if you look at the age spectrum and the gender of individuals with sleeplessness, there’s a large bum in menopausal women that menopause, premenopausal age range, female gender, about 2:1 incidence in women versus men in that age group is really a peak. |
| There were also things like what are called The Vaso-Motor Symptoms Of The Menopause period, hot flashes, night sweats, and a number of patients who started on the device have told us that they’ve noted significant reductions in some of these associated features of menopause that can lead to sleeplessness at night time. | ||
| 26:01 | So one trial that we want to move in to test out more specifically efficacy and safety with those types of symptoms were starting up some studies at this point in time. The other population that has expressed a lot of interest is headache sufferers, especially migraine headache sufferers, the application of cooling or different things that they had is one of the most common things that a migraine sufferer will try to do to try to give them some type of relief. | |
| And we’ve had several individuals who’ve been on the device that have found that the device has really able to terminate the evolution of a migraine episode to a much greater degree than if they weren’t using the device. And we’ve also had individuals who had longstanding chronic recurrent migraines who use it at night time for sleep, and they’ve actually surprisingly noticed a reduction and how often they’re having migraines during the daytime. | ||
| So that’s another area that we want to do some more testing in, do some pilot studies and some larger scale clinical trials because we think that’s an exciting area. Another area that we’ve started looking at, there’s a number of pediatric sleep clinicians that treat individuals or treat kids with Attention Deficit Hyperactivity Disorder, ADHD. Right now, they use stimulant medications and things to keep them focused and awake during the day time. But these individuals may have sleep disruptions and sleep fragmentation and sleep deprivation that might exacerbate some of their daytime ADHD symptoms. So we have a trial that’s underway now at a pediatric sleep center where they’re using it to improve sleep and ADHD kids to see if that has associated improvements in their waking daytime performance. | ||
| So those are a few areas and we have other areas that continue to come at us, but those are some of the ones we’re focused on right now. | ||
| Dan Pardi: | 27:25 | How loud is the device sitting by your bedside? |
| Eric Nofzinger: | The divine three relies on Thermo electric cooling. That silent cooling that produces no noise whatsoever, but it does generate a little bit of heat. And so we have to have a small fan in the device, just like your computer might have a fan inside of it to get rid of some of the excess waste heat in a computer. That fan noise has a little bit of a background noise. A lot of people liken it to the use a sound machine. It’s actually not as loud as some of the sound machine Might have that’s out there. It’s about on the level or individuals with obstructive sleep apnea syndrome and they use CPAP machines. It would be kind of on the range of a background noise for that. | |
| Dan Pardi: | 27:33 | Does the tube come out the top of the mask, so going behind your head? |
| Eric Nofzinger: | Correct. We’re very fortunate because most of our engineers came from the CPAP treatment world and designing CPAP Masks and it’s much more challenging to get a comfortable CPAP mask because you’re interfering with the airway. You’ve got to have something over the nose. And you do have post management issues so our engineers are very familiar with how to design products that are optimal for sleep. | |
| So in this instance it was recognized very early on that the best configuration was to have the tubing come out the top of the device and then it actually just lays on the pillow and on the bed at nighttime when somebody is sleeping. But that’s the most comfortable position. It allows individuals to toss and turn if they need to. Obviously once you’re asleep you’re really not aware of any tube or anything else going on. | ||
| Dan Pardi: | 29:00 | I would also be interested to test it for napping. The days where I feel like I’d like to take a nap, I don’t usually have enough time for that. So if you could get to sleep faster within the 20 to 30 minutes that you have, if I have any time, that’s about it. That would be quite interesting. And I wonder if even if you didn’t fall asleep simply the cooling felt restorative- |
| Eric Nofzinger: | Right. | |
| Dan Pardi: | 29:20 | So daytime usage without sleep. Does that have a meditation like clearing of your mind? |
| Eric Nofzinger: | We did have a study that actually was done at SRI and they’re very comfortable with the assessment to the autonomic nervous system and parasympathetic measures. We have them do a study just during daytime use and the subjective experiences were exactly that. It did have this relaxing meditation like quality that just used the device for about 30 minutes and the middle of the day they actually, these were insomnia individuals and I believe it was 80% of the individuals that use it during the day actually fell asleep, which is unusual for most individuals with insomnia. They’d tried to take a nap during the daytime. They wouldn’t be able to do that, so their subjective experience was very similar to what you’re describing | |
| Dan Pardi: | 29:46 | A lot. One, this is great, Eric. It’s really nice to hear the trajectory of how you got into sleep. Some of the problems that you identify as in terms of the detection methods we use particularly in insomniacs, you then used functional imaging to detect hypofrontality this hyper activity in the frontal cortex is during sleep and insomniacs. That then leads to the sluggishness, the hypofrontality the next day and how this has led to this product now that people can benefit from that knowledge. |
| I’ll put it in our show notes where people can find you. I really appreciate the work that you’ve done and coming onto our show to talk about it. | ||
| Eric Nofzinger: | 30:06 | Well, thank you very much. It’s been a great opportunity. I have been enjoying talking with you and hopefully providing a little bit of knowledge and education about what we think is we’re revolutionary technology in this field that hasn’t been in existence previously. So thank you for the opportunity. |
The post Can We Beat Insomnia by Cooling the Racing Mind? Podcast with Dr. Eric Nofzinger appeared first on humanOS.me.